Heavy drinkers may be at risk of alcoholic pancreatitis. Learn more about how alcohol damages the pancreas, and the relationship between alcohol and pancreatitis. The post Can alcohol cause pancreatitis? first appeared on Ardu Recovery Center, Provo, Utah.
Can alcohol cause pancreatitis?
Mina Draskovic, B.Psy., reviewed this content for accuracy on December 12, 2023
Ever wonder what a night of drinking does to your pancreas? Excessive drinking has been directly linked to inflammation of the pancreas, which is more commonly known as pancreatitis.�
Klockhov, et. al. revealed that �recurrent bouts of acute pancreatitis are associated with progression to chronic pancreatitis and are more common in chronic abusers of alcohol.�
Table of Contents
Alcohol-induced inflammation damages pancreatic cells and disrupts the normal functioning of enzymes, leading to this painful and potentially serious condition.�
This chronic inflammation sparked by one too many drinks can wreck your health. If you or� someone you know is struggling with alcohol addiction, help is available.�
Our rehab center in Provo, Utah can help you break the cycle of alcohol addiction through comprehensive treatment programs. These include medically monitored alcohol detox, psychotherapy, group support, and aftercare planning.�
What does the pancreas do?
The pancreas is a long, flat organ that is vital to the digestive and endocrine systems. It is both an organ as well as a gland.�
As an organ, the pancreas performs exocrine functions and produces digestive enzymes such as amylase, lipase, and protease. These enzymes are released into the small intestine to help break down carbohydrates, fats, and proteins, and absorb nutrients from ingested food.As a gland and part of the endocrine system, the pancreas produces and releases hormones. The pancreas contains clusters of cells called the islets of Langerhans. They produce hormones such as insulin and glucagon that help regulate blood sugar levels and signal the release of glucose (sugar) into the bloodstream.Proper functioning of the pancreas is paramount for overall well-being. It plays the following vital roles:
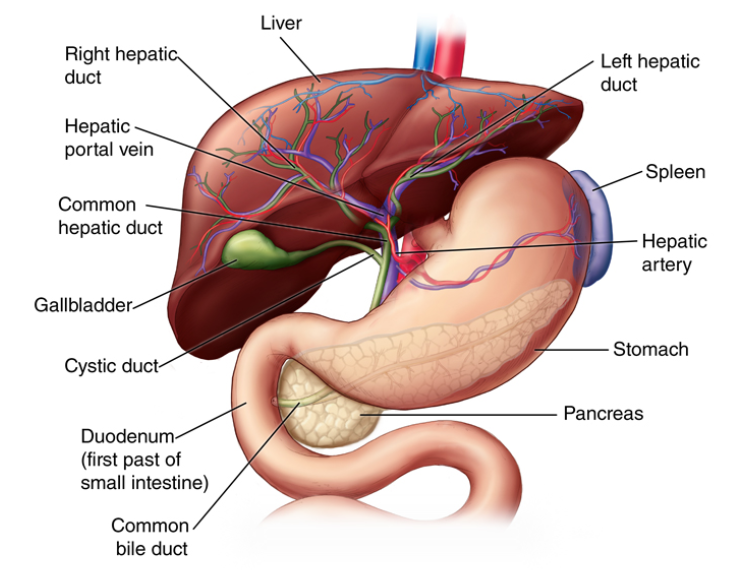
The pancreas regulates blood sugar. A healthy pancreas is important for preventing diabetes, a condition characterized by impaired insulin function and elevated blood sugar levels.The pancreas helps absorb nutrients. Proper digestion of food by pancreatic enzymes ensures the body receives essential nutrients for energy and overall health.The pancreas maintains metabolic balance. It regulates the production of insulin, which helps regulate metabolism and blood sugar levels while impacting fat storage, energy utilization, and overall metabolic balance.�Pancreatic bicarbonate neutralizes acidic chyme (partially digested food) in the stomach. This helps create an optimal environment for pancreatic enzymes to function and maintain the acid-base balance in the digestive system.The pancreas also plays a key role in immune system regulation. Islets of Langerhans produce insulin and glucagon that not only regulate blood sugar but also have immunomodulatory effects that influence the body�s defense mechanisms.�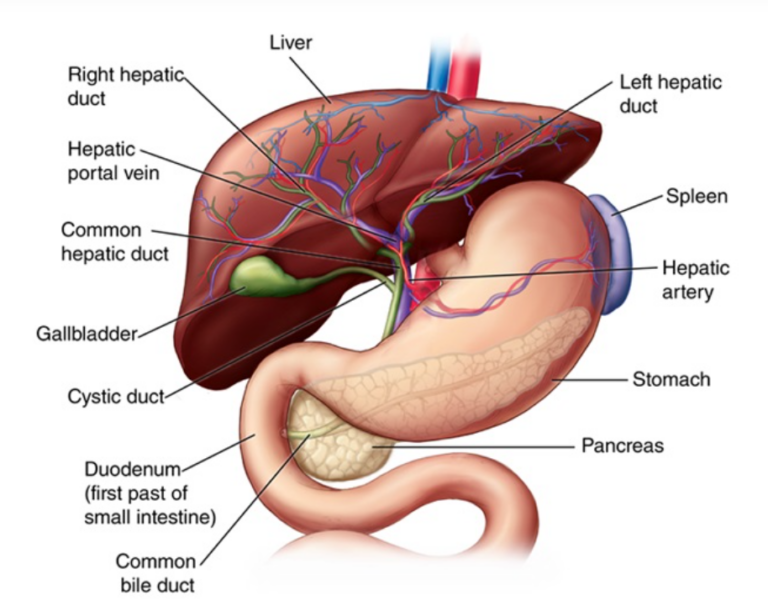 The pancreas. Source: https://www.drpapoulas.com/condition-procedure/pancreatic-diseases/
The pancreas. Source: https://www.drpapoulas.com/condition-procedure/pancreatic-diseases/
The pancreas collaborates with the liver in the breakdown and absorption of nutrients. Together, they ensure effective digestion, nutrient utilization, and maintenance of metabolic balance in the body.�
Here�s how these two powerhouse organs team up:
Pancreatic enzymes collaborate with bile from the liver to break down food for optimal nutrient absorption.�The common bile duct connects the liver, gallbladder, and the pancreas. Bile and pancreatic enzymes travel through it before entering the duodenum. This is where partially digested food mixes with digestive juices from the pancreas and bile from the liver to kickstart digestion.�The pancreas and liver work in tandem to regulate blood sugar levels. The pancreas releases insulin, while the liver stores and releases glucose.Together, they contribute to overall metabolic balance. The liver engages in generating glucose and storing glycogen, while the pancreas influences fat storage and energy utilization.These two organs are incredibly important for your health, so treat them with care. Many people suffer from impaired liver or pancreas function, especially those who indulge in regular binge drinking or develop alcohol dependency over years of heavy drinking.�
Alcohol can wreak havoc on your liver, and it doesn�t treat your pancreas any better.
What are the effects of alcohol on the pancreas?
The pancreas is extremely susceptible to the toxic effects of alcohol. While low to moderate alcohol consumption may not immediately raise alarms, chronic alcohol abuse can cause a myriad of detrimental effects on your pancreas.�
Here are some of the most notable effects:
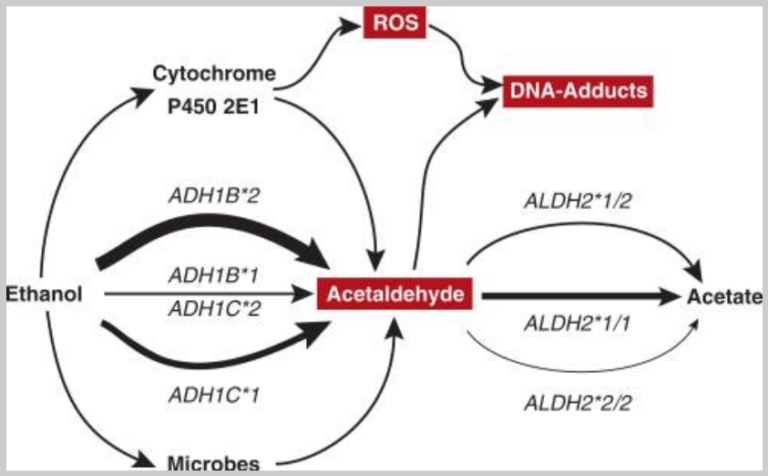
Chronic alcohol consumption triggers inflammation in the pancreas, which develops into a condition known as alcoholic pancreatitis.�Increased inflammation triggers oxidative stress. The metabolism of ethanol (alcohol�s main constituent) generates a variety of toxic byproducts, including reactive oxygen species (ROS). Through the process of oxidation, these harmful molecules damage pancreatic cells.�The production of vital digestive enzymes suffers under the influence of alcohol. Heavy drinking can disrupt the breakdown of food and hinder your body�s ability to absorb essential nutrients (one of the many ways alcohol depletes your body of nutrients).Continued alcohol intake may lead to pancreatic fibrosis, a condition where healthy tissue is replaced by scar tissue. This compromises the pancreas�s structural integrity and functionality.Heavy alcohol consumption increases the risk of pancreatic cancer. In general, alcohol is a trigger for tumor development.Alcohol-induced pancreatic damage can lead to pancreatic edema�your pancreas swells due to excessive inflammation.�In severe cases, alcohol-related pancreatitis can progress to pancreatic necrosis where areas of the pancreas experience cell death.�Your liver thrives when you ditch alcohol, and the same is true with the pancreas. When you take alcohol out of the equation, your pancreas can gradually heal, reduce inflammation, restore enzyme production, and reclaim its pivotal role in digestion.�
What are you waiting for? Contact Ardu and start your journey to recovery today.
What is pancreatitis?
Pancreatitis is an inflammatory condition of the pancreas. This potentially life-threatening and often chronic disease disrupts the delicate functions of the pancreas, leading to a wide range of complications, and in some severe cases, death.
Here�s how pancreatitis unfolds:
A trigger prompts premature activation of pancreatic enzymes.�When activated in the small intestine, pancreatic enzymes aid digestion. Pancreatitis causes these enzymes to become prematurely activated, leading to autodigestion where enzymes start attacking pancreatic tissue.Your body�s natural response to threat is to increase inflammation. The immune cells send first responders to the �crash site,� fueling inflammatory processes and causing swelling.�The inflammation extends to blood vessels. More inflammatory cells are released, impairing blood flow to the pancreas.The combination of enzyme activity, immune response, and compromised blood flow causes extensive damage to pancreatic tissue. The damage can be mild, acute inflammation, or severe and chronic.The damaged pancreas may develop pseudocysts (fluid-filled sacs) or areas of necrosis (dead tissues) that further impede pancreatic function and lead to more complications.�In severe cases, inflammatory mediators and enzymes enter the bloodstream and travel to other organs where they spread inflammation.�Chronic inflammation remains in the pancreas, leading to pancreatitis and often resulting in irreversible damage. The pancreas may not be able to produce precious digestive enzymes and insulin.�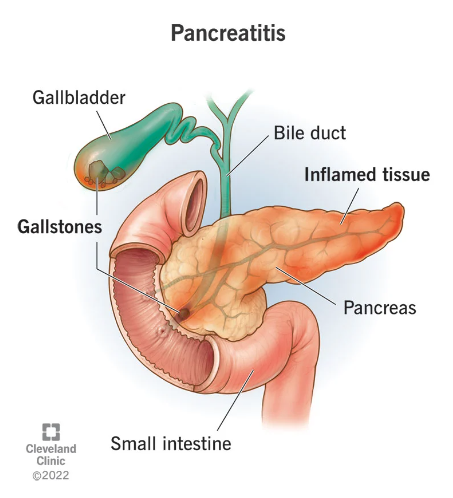 Source: https://my.clevelandclinic.org/health/diseases/8103-pancreatitis
Source: https://my.clevelandclinic.org/health/diseases/8103-pancreatitis
Inflammation can be triggered by many different factors.�
Gallstones can obstruct the pancreatic duct, impeding the flow of enzymes and causing inflammation.�Certain medications can cause chronic inflammation in the body that leads to pancreatitis.�Infections can be a trigger for inflammation.�Physical trauma to the abdomen (injury or surgery) can be a factor.Elevated levels of triglycerides in the blood can contribute to pancreatitis.Autoimmune disorders, where the immune system mistakenly attacks the pancreas, can lead to inflammation.Hypercalcemia, or elevated levels of calcium in the blood, can be associated with pancreatitis.People with cystic fibrosis may be at an increased risk due to thickened secretions affecting the pancreas.Hereditary factors and genetic predisposition can play a role in relative susceptibility to pancreatitis.Obesity increases the risk of pancreatitis and can lead to more severe complications.Excessive alcohol consumption is one of the most prevalent causes of pancreatitis. Apart from triggering inflammation, alcohol inflicts damage to the cells of the pancreas.�While acute pancreatitis refers to a single instance of inflammation, excessive alcohol use often leads to persistent inflammation of the pancreas. Alcohol-induced pancreatitis is one of the most common conditions of which alcohol is the primary trigger.�
How does alcohol cause pancreatitis?
Heavy, regular drinking impairs normal pancreatic function in many ways. With that being said, chronic inflammation is the true culprit of pancreatitis.�
The pancreas will try to compensate for the damaging impact at first, but the more you drink, the more exhausted your pancreas becomes. Soon, it is unable to function properly.
Here�s what happens when you flood your pancreas with booze:
Alcohol is metabolized in the liver and partly in the pancreas where it generates toxic byproducts such as acetaldehyde. Acetaldehyde causes DNA damage and impairs cell function (Mizumoto, et. al.). Your pancreatic cells try to compensate by producing more digestive enzymes and insulin.�Acetaldehyde and other alcoholic metabolites cause a blockage of pancreatic fluid secretions. A 2010 study suggests that acetaldehyde is toxic to pancreatic acinar cells, the type of pancreas cell that produces digestive juices. Unable to leave, digestive enzymes build up inside the pancreatic duct, leading to premature activation and autodigestion.�Damaged pancreatic cells trigger the release of proinflammatory mediators. Alcohol is damaging to your immune system, and it definitely won�t help with the immune response to inflammation.�Chronic inflammation in the pancreas leads to pancreatic necrosis, fibrosis, and calcification. Gradually, scar tissue and calcium accumulate inside the organ, hindering its ability to produce digestive enzymes and glucose-regulating hormones. The result is a case of chronic pancreatitis.Repeated bouts of acute inflammation from direct ethanol effects slowly damage the pancreas beyond repair. Some experts say that mild or occasional drinking poses little risk, while heavy consumption burns out the organ.�
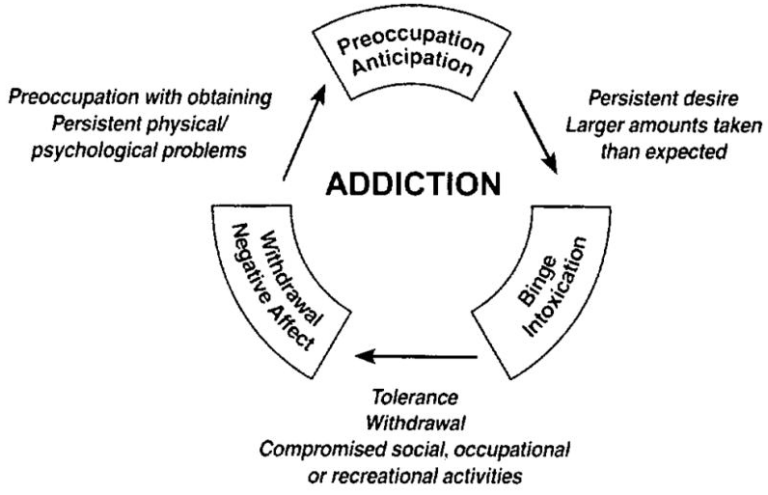
We say it�s time to ditch the bottle. It isn�t always easy to quit, especially if addiction has sunk its claws into every aspect of your life. Many alcoholics will relapse and resume drinking, often in an attempt to curb withdrawal symptoms. Sadly, this only serves to perpetuate the cycle of addiction.�
Contact Ardu Recovery Center to get the alcohol counseling and treatment you need.
What are the signs of pancreatitis from alcohol?
Symptoms of alcohol-induced pancreatitis manifest similarly to other forms of pancreatitis. Like other types, alcohol-induced inflammation of the pancreas is extremely painful.�
Here are the symptoms of alcoholic pancreatitis:
Nausea and vomitingFeverRapid heart rateIntense abdominal pain, often radiating to the backTenderness of the abdomen, especially in the upper middle regionSwelling of the abdomenJaundiceClay-colored stoolShock or fainting (in severe cases)Pain from inflammation is a cardinal symptom in all forms of pancreatitis. In alcoholic pancreatitis, abdominal tenderness, and distention alongside nausea and increased heart rate are telling signs of the toxicity of alcohol.�
Did you know that alcohol is also toxic to your brain?
How much alcohol causes pancreatitis?
Apte et al found that �the risk of developing pancreatitis increases with increasing doses of alcohol, suggesting that alcohol exerts dose-related toxic effects on the pancreas.� Klockhov, et. al. revealed that acute pancreatitis �usually manifests in patients with over five years of ongoing, substantial alcohol use (~4-5 drinks daily) and only rarely occurs from isolated binge drinking.��
Vonlaufen, et. al., however, offer a different take, explaining that �less than 10 percent of heavy alcohol users (180 g/day or about 15 drinks per day for 10 to 15 years) eventually develop clinically overt alcoholic pancreatitis.�
Here�s what you need to know about the relationship between alcohol and pancreatitis:
Any amount of alcohol can potentially cause pancreatitis in people who are susceptible or suffer from other forms of pancreatic disease. The risk rises sharply with excessive amounts and longer duration of consumption.Women appear to be at greater risk than men with comparable levels of alcohol consumption. According to a 2015 study, �there is a threshold effect for acute pancreatitis in women at the level of up to 40 g/day.�The amount of alcohol that triggers pancreatitis differs from person to person based on genetics, health conditions, and lifestyle factors.If you have a problem with binge drinking or find yourself unable to quit, there�s a high probability that you are either struggling with addiction or are at risk for developing a problem. Read our guide to the tell-tale physical symptoms of alcohol addiction.
How does alcohol withdrawal affect pancreatitis?
Alcohol withdrawal can exacerbate inflammation in acute pancreatitis.�
Here are some of the reasons why:
Withdrawal leads to increased secretion of pancreatic digestive enzymes. This abundance of enzymes builds up inside pancreatic ducts rather than being appropriately released into the small intestine. The backed-up enzymes then digest and damage pancreatic tissue, exacerbating inflammation.During withdrawal, the sphincter of Oddi (the muscular valve regulating the flow of enzymes) tightens and spasms abnormally. This closes the pancreatic duct and causes trapped enzymes to accumulate, triggering autodigestion.People going through alcohol withdrawal become super sensitive to cholecystokinin, the key hormone that stimulates the pancreas to produce digestive enzymes. This hormone triggers exaggerated enzyme secretion by pancreatic cells in response to eating. Overproduction of enzymes in the pancreas leads to autodigestion.Alcohol withdrawal activates inflammatory pathways inside pancreatic tissue. This amplifies the inflammatory response and associated cell damage, exacerbating the severity of acute pancreatitis.It�s important to manage withdrawal early on, especially in hospitalized alcoholic pancreatitis patients. The quicker you intervene, the lower the risk of life-threatening delirium tremens or alcohol withdrawal syndrome.
Our medical detox program can help you get through the initial stages of withdrawal, while our alcohol rehab program teaches you how to rewire your patterns, body, and brain to live an addiction-free life.�
What is the life expectancy for a person with alcoholic pancreatitis?
Alcoholic pancreatitis can severely shorten a person�s lifespan. Research shows that around half of patients with alcohol-related pancreatitis die within 20 years of disease onset.�
Only 20 percent of deaths occurring before a patient�s life expectancy are attributed to pancreatitis or its complications; most of these deaths are attributed to the toxic effects of alcohol or smoking on other organs such as the liver. (Apte, et. al.)
A 2023 study revealed that patients with chronic alcoholic pancreatitis have a 95.5% one-year survival rate after surgery. Long-term prognosis tends to decline significantly with 63.5% of patients living 10 years post-operation.�
How is alcoholic pancreatitis treated?
This complex condition requires a comprehensive treatment plan that tackles substance use, chronic pain, nutrition, and other factors.�
There are several key aspects to treating alcoholic pancreatitis:
Eliminating alcohol and smoking is essential to prevent further damage and inflammation of the pancreas.�Strong pain medications may be used for severe pain flare-ups. Doctors often use nerve blockers or other techniques to reduce severe pancreatitis pain.Aggressive hydration aids the recovery process. Vigorous fluid therapy through IV hydration helps stabilize blood pressure and circulation.Many patients struggle with eating due to nausea or malabsorption. It�s important to provide balanced nutrition through dietary changes or supplement drinks to prevent further complications.Enzyme levels require close monitoring and adjustment. Digestive enzymes taken orally help with the breakdown of food.�For acute pancreatitis, treatment usually involves hospitalization where patients can be closely monitored for signs of serious complications.�Procedures such as drainage, debridement, or partial pancreas removal may help alleviate persistent fluid collections, duct obstructions, or uncontrolled pain.Some people with acute pancreatitis have an alcohol dependency and need support to stop drinking. If this is you, contact Ardu today and start your recovery journey.
Ardu Recovery Center
Recovery is a personal journey. Rather than taking a one-size-fits-all approach, the Ardu team develops customized treatment plans tailored to your specific needs and goals.�
Inpatient treatment at our residential facilities surrounds you with 24/7 support. Outpatient treatment programs, such as partial hospitalization and intensive outpatient programs, offer flexible solutions to maintain your home and work routines or receive treatment while in a sober living facility.
With psychotherapy and other modalities, you learn healthy coping skills so you aren�t tempted to rely on alcoholic beverages. A variety of therapeutic approaches�from cognitive behavioral therapy and motivational interviewing to dialectical behavioral therapy�allow you to find the modality that resonates with you.
If you have a co-occurring mental health disorder, our dual diagnosis treatment program and mental health treatment plan can help you deal with alcohol addiction as well as other mental health issues.�
Alcoholism and mental health issues often go hand in hand, and we do everything in our power to help you find your way back to wellness. Our comprehensive recovery program can aid you in restoring a healthy, well-balanced lifestyle.
Alcohol and pancreatitis FAQ
Can alcoholic pancreatitis cause death?
Alcoholic pancreatitis can lead to death, both directly from disease progression and indirectly through systemic complications. As previous studies have shown, 50% of patients die within 20 years of diagnosis, and over a third sooner than the general population. Just 20% of these premature deaths directly result from chronic pancreatic injury.
The immune, endocrine, and digestive dysfunction induced by alcoholic pancreatitis can leave chronic pancreatitis patients severely debilitated and vulnerable to a cascading decline in health. Acute flare-ups of alcohol-related inflammation can result in organ failure, uncontrolled bleeding, infection, and other life-threatening issues. Over time, chronic pancreatic damage also raises the risk of diabetes, malnutrition, cancer of the gastrointestinal tract, and liver disease.
How long after drinking does pancreatitis start?
An acute pancreatitis episode can start just 48 hours after a binge drinking session. It often requires five or more years of continued alcohol intake for chronic alcohol-induced pancreatic injury from recurrent attacks to accumulate. Both acute and chronic alcohol-induced pancreatitis leave patients vulnerable to frequent acute flare-ups. The accumulation of inflammation that alcohol triggers can quickly spark swelling, pain, and systemic complications due to the destruction of pancreatic tissue over time.�
How does alcohol damage the liver and pancreas?
The metabolism of ethanol generates significant oxidant stress which inflames tissues through its toxic byproducts. Alcohol causes protein deficiency, impairs protein response, and causes fatty liver, fibrosis, and cirrhosis, compromising cell integrity in both the liver and pancreas. Chronic ethanol administration can lead to alcoholic liver disease over time.
Specialized pancreatic stellate cells activate and release collagen scar tissue when chronically stimulated. Both vital organs suffer substantial structural and functional damage from the effects of alcohol consumption.�
How do I know if alcohol has damaged my pancreas?
There is a wide range of characteristic symptoms that indicate pancreatic damage from alcohol. These include:
�Abdominal painLoose oily stoolsUnintentional weight lossVomitingLow-grade feverNauseaBlood labs measure elevated pancreatic enzymes and tests like CT scans reveal ductal calcifications and parenchymal scarring that is indicative of alcohol damage.
If chronic pancreatitis patients display these symptoms and indicators, it may mean that pancreatic tissue damage from alcohol has occurred.
Can the pancreas repair itself?
The pancreas has remarkable regenerative capabilities. When given enough time and care, it can undergo a healing process, particularly when mitigating factors such as alcohol use disorder (AUD). Its repair also depends on the severity of alcohol dependence, the type of alcohol consumed, and the extent of long-term alcohol consumption.�
Things like hereditary factors, environmental factors, and lifestyle choices can hinder the pancreas� healing process.�
It�s important to adopt a healthy lifestyle that will combat the development of pancreatitis. Make sure you incorporate clinical recommendations from your doctor and support your pancreas� natural repairing process.�
Will pancreatitis go away if I stop drinking?
When you put an end to chronic alcohol consumption, you give your pancreas a chance to heal. This means acute or chronic cases of pancreatitis may potentially be resolved.�
It�s important to address the detrimental effects of alcohol metabolites�such as acetaldehyde and reactive oxygen species. Address biological and environmental factors so your pancreas can recover from recurrent attacks.
Can you ever drink alcohol again after pancreatitis?
Post-pancreatitis drinking (regardless of the amounts of alcohol) may trigger significant harm thanks to vulnerability caused by previous inflammatory damage. There is a substantial risk of experiencing recurrent episodes of pancreatitis even after years of abstinence.�
If you suffered from alcoholic pancreatitis in the past, even an occasional drink might trigger some of the following:
Painful pancreatitis attacksAdvanced pancreatic destructionDuctal blockages that require surgical interventionIncreased enzyme production deficiencyMalnutritionDiabetesSevere disabilityExtended hospitalization staysPeople with a history of diagnosed pancreatic inflammation should abstain from the consumption of alcohol. To preserve precious pancreatic integrity, enzyme output, glycemic control, nutritional status, and overall health and prevent acute attacks of pancreatitis, work towards lifelong sobriety and vitality.�
Do most alcoholics get pancreatitis?
According to research, less than 5% of chronic, heavy drinkers get diagnosed with clinical pancreatitis.�
In a population of 10%-15% of heavy drinkers, 2%-5% of all PC cases could be attributed to alcohol consumption. However, as only a minority (less than 10% for pancreatitis and 5% for PC) of heavily drinkers develops these pancreatic diseases, there are other predisposing factors besides alcohol involved. (Herreros-Villanueva, et. al.)
Researchers have analyzed predisposing factors such as alcohol metabolism, smoking, dietary co-factors (e.g., high-fat content, presence of infections), and calcium levels that may promote pancreatic cell injury. With that being said, no firm causative links have been found to explain why most drinkers avoid developing pancreatitis despite their alcohol-drinking habits.
How can I protect my pancreas from alcohol?
To protect your pancreas, it�s best to limit drinking�or better yet, cut out alcohol altogether. The effects of ethanol on the human pancreas are toxic and destructive, so even acute episodes of binge drinking may inflict damage.�
It�s important to maintain a balanced, low-fat diet, stay properly hydrated, and promptly treat any infections or conditions that could act as a trigger factor. It�s always best to seek medical care if you�re concerned about potential pancreatic symptoms.�
While the human body can bounce back from acute attacks if they are spaced apart, consistent chronic damage can lead to loss of function.
Resources
Klochkov, A. (2023, May 16). Alcoholic Pancreatitis. StatPearls � NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537191/
Mizumoto, A., Ohashi, S., Hirohashi, K., Amanuma, Y., Matsuda, T., & Muto, M. (2017, September 10). Molecular Mechanisms of Alcohol to Acetaldehyde-Mediated Carcinogenesis in Squamous Epithelium. International Journal of Molecular Sciences. https://doi.org/10.3390/ijms18091943
Vonlaufen, A. (2007). Role of Alcohol Metabolism in Chronic Pancreatitis. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860433/
Apte MV, Pirola, R. C., & Wilson J. S. (2010, November 23). Mechanisms of alcoholic pancreatitis. Journal of Gastroenterology and Hepatology. https://doi.org/10.1111/j.1440-1746.2010.06445.x
Samokhvalov, A. V., Rehm, J., & Roerecke, M. (2015, December 1). Alcohol Consumption as an Additional Risk Factor for Acute and Chronic Pancreatitis: A Systematic Review and a Series of Meta-analyses. EBioMedicine. https://doi.org/10.1016/j.ebiom.2015.11.023
Wilson, G. C., Turner, K. M., Delman, A. M., Wahab, S. A., Ofosu, A., Smith, M. T., Choe, K. A., Patel, S. H., & Ahmad, S. A. (2023, March 15). Long-Term Survival Outcomes after Operative Management of Chronic Pancreatitis: Two Decades of Experience. Journal of the American College of Surgeons. https://doi.org/10.1097/xcs.0000000000000575
Herreros-Villanueva, M., Hijona, E., Ba�ales, J. M., Cosme, A., & Bujanda, L. (2013). Alcohol consumption on pancreatic diseases. World Journal of Gastroenterology: WJG, 19(5), 638-647. https://doi.org/10.3748/wjg.v19.i5.638
Further reading
How much alcohol is too much to drink?
How do I know if I have an alcoholic personality?
What are the health risks of alcohol for men?
Can alcohol mess with birth control?
How does heavy drinking impact the brain?
Is beer the cause of the �beer belly�?
What is a high-functioning alcoholic?