In honor of National Caregivers Month, Bob Harley shares his experience caring for his wife who had Alzheimer’s disease. He shares the importance of education and the tips and tricks he learned that can... The post Bay Area spouse...
In honor of National Caregivers Month, Bob Harley shares his experience caring for his wife who had Alzheimer’s disease. He shares the importance of education and the tips and tricks he learned that can help make caring for your loved one a little easier.
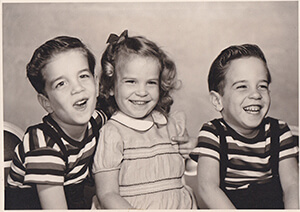
Childhood friends
Adrienne Harley was a triplet, and the only girl. In the fourth grade her brothers became friends with Bob. Of course, at that age, girls and boys don’t often play together so while the boys became fast friends, Adrienne spent her time with other girls.
As teenagers Adrienne and Bob were never interested in each other. Adrienne attended the local all-girls school while her brothers and Bob attended the all-boys school. Adrienne dated Bob’s best friend, and occasionally she and Bob would double date.
The night before the all-girls school prom, Adrienne’s then boyfriend got sick, and her brothers suggested she take Bob. The pair agreed and began what would be a lifetime together. “We dated on and off during college,” said Bob. “Then it became on and we were married the year after we graduated. We have two boys and were married for 56 years.”
Family life
Adrienne was an artist who loved painting and making jewelry. She and her family spent many weekends and summers at their houseboat. “We took the kids to the library on Thursday to get a bag of books,” said Bob. “We’d head to the Delta on Friday and spend the weekend there. There were no electronics, no cell phones, no TV. There was a lot of interaction, a lot of reading and game playing. More than one deck of Uno found its way into the water as I would get frustrated.”
With a degree in biology, Adrienne became a licensed medical technologist and spent many years working in labs. She took a few years off to have children, and when they were old enough, she returned to work part time. She finished her career working at an eye center as the assistant to the primary physician.
Memory problems
Adrienne began to notice she was having problems with her memory and, in 2015, took it upon herself to see her doctor. After an evaluation, she was diagnosed with mild cognitive impairment (MCI). MCI is an early stage of memory loss or other cognitive ability loss (such as language or visual/spatial perception) in individuals who maintain the ability to independently perform most activities of daily living.
To help her brain Adrienne did what she could to strengthen her memory. “She went to a number of different classes,” said Bob. “She became involved with computer and memory games. Every night we’d have a game of Mexican Train before dinner. Life went along.”
Re-evaluated
By 2017 Adrienne could tell her memory was getting worse. She went in to be re-evaluated, hoping there were new medications that could help. Sadly, at that time there were not.
Currently there are two new treatments available to people in the early stages of the disease. In 2021 the U.S. Food and Drug Administration (FDA) approved Aducanumab (Aduhelm®)) which was the first therapy to reduce cognitive and functional decline in people living with early Alzheimer’s.
Then, in early 2023, Lecanemab (Leqembi®) received FDA approval. Both of these treatments are anti-amyloid treatments. They work by attaching to and removing beta-amyloid, a protein that accumulates into plaques, from the brain. Each works differently and targets beta-amyloid at a different stage of plaque formation.
Retaking the driving test
Alzheimer’s disease typically progresses slowly in three stages: early, middle and late (sometimes referred to as mild, moderate and severe in a medical context). Since Alzheimer’s affects people in different ways, each person may experience dementia symptoms — or progress through the stages — differently.
After Adrienne’s doctor visit in 2017, she was told she was in the early stage of the disease. Because of her updated diagnosis, her doctor informed them that he was required to tell the Department of Motor Vehicles (DMV) of her diagnosis. “The neurologist told us it was no big deal,” said Bob. “What the neurologist didn’t say was that he had checked the box, ‘I advised her not to drive.’ The DMV suspended her license.
“[She went and took the driving test] but didn’t pass. I think I would be nervous about taking the driving test. We all get sloppy, and I think that was why she failed. We sent her to driving school, and she passed with flying colors.”
Hiding the keys
Determining when someone can no longer safely drive requires careful observation by family and caregivers. Things like forgetting how to locate familiar places, hitting curbs and driving at an inappropriate speed are all signs that it’s time to stop driving.
By 2018, Adrienne was unable to find her way to familiar locations, including her home. At first, Bob, with Adrienne’s consent, put a GPS tracker on her phone so he would know where she was if she got lost. Eventually it became clear that Adrienne needed to stop driving.
“It was an easy passage,” said Bob. “I would just say, ‘Oh, I’ll take you shopping. I want to go anyway.’ Or ‘Oh, I’ll take you to the breakfast meeting with the ladies. There is a great path, and I want to go for a walk for an hour.’ There wasn’t an argument, but I did hide the car keys.”
Wandering
As the disease progressed, so did Adrienne’s symptoms. In 2019 a new one started and Adrienne began wandering. First around the house, waking up in the middle of the night to make food. Later she would try to leave home.
Alzheimer’s disease causes people to lose their ability to recognize familiar places and faces. It’s common for a person living with dementia to wander or become lost or confused about their location, and it can happen at any stage of the disease.
Six in 10 people living with dementia will wander at least once; many do so repeatedly.
“If I was gone, she’d be outside with the neighbor with a bag in her hands saying ‘Take me home to city.’” Said Bob. “She’d have a shoe, a blouse and whatever in the bag. Luckily the neighbor would not.”
At first Bob hired a caregiver when he needed to go out but eventually it reached a point where the family decided it was best for Adrienne to move into a care setting.
Birthday party
Adrienne continued to wander at the care settings, but sadly this meant many middle of the night falls. Bob would get calls at 3 a.m. to meet her at the emergency room. When she stopped eating, they moved her into hospice care.
For her 79th birthday, her sons decided to get the family together on a Zoom call. Despite all the effort, Adrienne didn’t seem aware of what was going on. The next day, the nurses called Bob and told him it was time. Adrienne died later that day.
Tips for caregivers
While Bob’s caregiving journey is over, he wants to share these tips with other caregivers.
Get educated about the disease. Start early, for both the caregiver and the person living with the disease.Take classesRead books or visit the Alzheimer’s virtual library Find resources on alz.org Don’t get angry. The person you love has a disease that they can’t control and isn’t their fault. It’s okay to be frustrated but you shouldn’t get angry with them. Don’t use the word “remember.” Tell the person living with the disease about past experiences instead of asking if they remember them. When reflecting on the past, Bob would tell Adrienne, “We had a good time boating with the boys, that was a lot of fun.” Utilize the latest technology. At the time of Adrienne’s diagnosis, Bob was able to put a tracker on her phone or in her purse. Today, there are even more ways technology can assist a caregiver. Things like motion detectors, or bedroom door alarms can help keep your loved one safe.Education classes
The Alzheimer’s Association offers several free education classes for caregivers to learn more about the disease and how to better help their loved ones. The Association frequently partners with organizations like Kaiser Permanente to help get necessary information and resources to a wider community.
Bob, who was a member at Kaiser, was able to take education classes at the local medical offices. “We went to a number of those classes and alz.org is one of the references,” said Bob. “It was an awakening for me. [You’ll learn to] understand the disease so that you don’t criticize the person [living with the disease]. [Instead], you learn different ways of dealing with them in a positive way.”
Join a support group
Bob also encourages caregivers to attend support groups. “They can learn ways to help them cope, and to know they aren’t alone,” said Bob. “There are other people going through this. Even though [when I went to the support group] I was in denial, I learned something.
“In my life, I was always the person who could take care of things and fix things. Well, you can’t fix this one, you can ride along and help but you can’t fix it. The reason I went back [to the support group was] because I thought maybe I could help others. I got some great questions and they said, ‘You really helped us by sharing the complete journey.’”
For more information on Alzheimer’s resources and to learn more about the disease visit our website at alz.org.
November is National Caregivers Month, honor a caregiver at alz.org/honor.
The post Bay Area spouse caregiver shares tips and resources for new family caregivers first appeared on Alzheimers and Dementia Blog - Alzheimers Association of Northern California and Northern Nevada.