A common question we get from prospective patients at Alzheimer’s Clinics is “I’ve heard of TMS, is this like that?”. In some ways yes, in many ways no. It is true that both TMS and TPS share the meaning...
A common question we get from prospective patients at Alzheimer’s Clinics is “I’ve heard of TMS, is this like that?”.
In some ways yes, in many ways no.
It is true that both TMS and TPS share the meaning of both their T and S, which are transcranial and stimulation, but the middle initial is what makes their mechanisms, effects, and treatment protocols so vastly different.
Transcranial Magnetic Stimulation
Transcranial Magnetic Stimulation, or TMS, is a neuromodulatory procedure which uses magnetic fields to stimulate targeted areas of the brain.
The first TMS device was designed by Anthony T Barker in 1985. TMS was originally designed as a tool for research. By stimulating different areas of the brain, we can learn more about what that region of the brain does. It was not until much later that they were discovered to have therapeutic potential.
A TMS device works by creating an electromagnetic field around a handpiece which is operated by the person providing the treatment. The handpiece is held over the patient’s head and the magnetic fields induce electrical charges within the brain. The field causes this electrical charge by altering transmembrane currents, resulting in depolarization or hyperpolarization of neurons.
The magnetic field can reach around 5cm deep into the brain, unless using a type of TMS called Deep TMS. Deep TMS is less commonly used.
TMS can be used to treat quite a few psychiatric and neurological conditions. By stimulating or inhibiting stimulation in areas of the brain which may be involved in the condition, some patients can gain relief from symptoms. TMS is typically used when more traditional treatment options have not worked.
There is published research that suggests TMS may be an effective treatment for:
Depression. Anxiety. Obsessive Compulsive Disorder. PTSD. Stroke rehabilitation. Schizophrenia. Multiple Sclerosis (MS).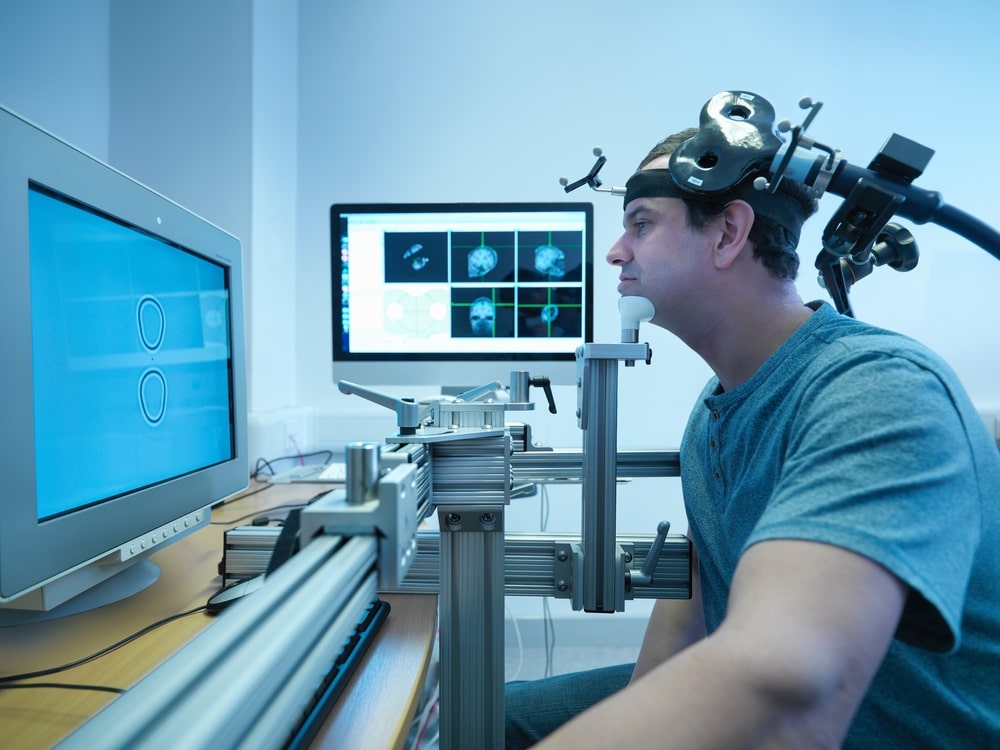

Transcranial Pulse Stimulation
Transcranial Pulse Stimulation (TPS) is a much newer treatment which involves passing high-frequency acoustic waves through the patient’s skull to stimulate targeted areas of the brain with millimetre accuracy. These acoustic pulses are similar to the shockwaves used in shockwave therapy, a highly researched and long standing treatment for many msk conditions.
Rather than stimulate neurons to fire, as TMS does, TPS induces neuronal mechanotransduction, which is when cells convert mechanical stimuli into biochemical signals. The neurons release growth factors such as BDNF, as well as nitric oxide. This is suggested to promote the formation of new blood vessels, helping blood get to areas of the brain it usually has difficulty with. It may also induce nerve regeneration.
There are currently nine published papers supporting TPS’ effectiveness in the treatment of Alzheimer’s dementia. Other research is currently looking at TPS for Parkinson’s, CTE and other types of dementia.
Where do the two differ?
Energy emitted
As previously mentioned, the most obvious difference between TMS and TPS is that TMS uses magnetic fields to influence the brain, whereas the TPS uses high-frequency acoustic pulses.
Type of stimulation
The second difference between the treatments is what is meant by “stimulation”. TMS causes neurons to fire by altering transmembrane currents. By increasing the rate at which neurons in that specific area of the brain are firing during treatment the therapeutic effect is achieved.
TPS does not cause neurons to fire. The momentum of the waves create slight movements in the cells they pass, stretching and deforming them and temporarily increasing their permeability to ions and certain molecules, as well as inducing the release of growth factors and other beneficial chemicals. The therapeutic effect of TPS is thought to be due to the release of these chemicals as well as increases in cerebral blood flow.
Tissue heating
TMS causes a small amount of tissue heating when used. This is typically less than 1°C, so is unlikely to cause damage to brain tissue, but it is a factor that the practitioner needs to consider when providing the treatment. Brain implants such as aneurysm clips and stimulation electrodes can heat up quickly during TMS.
Because of the nature of the energy emitted during TPS, tissue heating is not a concern. Any heating caused would be almost immeasurable and will have no effect on brain tissue or the patient.
Treatment depth & focal point
The maximum treatment depth of TMS depends on how deep the magnetic field of the device penetrates when held against the skull. This is typically around 5cm. A type of TMS called deep TMS, which is less commonly used, can reach deeper areas of the brain. The treatment area is also typically broad in TMS treatments, as any neuron within the magnetic field will be influenced.
TPS can reach slightly deeper into the cortex, up to 8cm. Similar to focused shockwave therapy, the strength of the acoustic waves in TPS are not strongest at the source, but rather at the treatment area. Because of this the energy can be focused with millimetre accuracy at a targeted brain area and minimise effects on surrounding tissue.










