In this protocol, we'll explore everything you need to know about chocolate toxicity in dogs, one of the most common veterinary emergencies. The post Chocolate Toxicity in Dogs – Clinical Protocol appeared first on Animal Emergency Australia.
In the world of veterinary emergency, chocolate toxicity in dogs stands out as a recurring theme during any time of year, but especially throughout the holiday season. And with Christmas just around the corner, we all understand the allure of this delectable treat, but it’s crucial to be aware of the potential risks and the importance of prompt action for pets that have indulged.
In our chocolate toxicity protocol, we’ll explore everything you need to know about chocolate toxicity in dogs. This includes exploring the various factors that influence its severity as well as the signs and symptoms to be aware of. We’ll also outline the steps veterinary professionals can take to navigate this common emergency scenario effectively. By staying informed and spreading awareness, we can ensure that any case of chocolate toxicity in dogs ends in the best possible patient outcome.

Pathophysiology of Chocolate Toxicity in Dogs
Theobromine is the predominant methylxanthine in the cocoa bean, along with caffeine in lower concentrations. Caffeine is also present in the coffee bean (and its by-products), and in fatigue-combating medications. Chocolates of all kinds are readily available and highly palatable, attracting animals to the product.
All animals can be affected by methylxanthine toxicosis, however, dogs are most commonly affected due to their indiscretionary eating habits and easy access to an owner’s foods or medications. Methylxanthines act through inhibition of cellular phosphodiesterase, increasing intra-cellular cyclic adenosine non-phosphate, enhancing the release of catecholamines epinephrine and norepinephrine.
Methylxanthines are competitive antagonists of cellular adenosine receptors and cause an increased entry of calcium into and inhibit calcium sequestration by the sarcoplasmic reticulum, increasing muscle contraction. The overall clinical picture is due to the neurological and cardiac stimulatory effects, along with gastrointestinal signs from local irritation.
Methylxanthine Toxic Dose Range
When calculating exposures, the combined total of theobromine and caffeine are determined to establish a total dose of methylxanthine ingested. When it is a mixed product (e.g. trail mix), or the dose consumed is unknown, always calculate based on worst-case scenario. Using a chocolate toxicity calculator can be a quick and easy guide to determining the level of toxicity.
Mild clinical signs (e.g. V+/D+) : 20-40mg/kg Severe clinical signs (e.g. tremors, arrhythmias): 40-50mg/kg Life-threatening clinical signs (e.g. seizures, death): >60mg/kgOnce ingested, methylxanthines are readily absorbed from the gut, however, the absorption and gastric emptying can be slowed from the fat composition of most chocolate products. Clinical signs generally occur within 6-12 hours of ingestion, but may be seen within 1-4 hours dependent on dose and type consumed.
The half-life of theobromine is 17.5hrs and caffeine 4.5hrs. Theobromine’s extended half-life is attributable to its enterohepatic re-circulation (returning to the circulating bloodstream via the portal vein after uptake in the ileum). There is also potential for prolonged clinical signs due to reabsorption through the urinary bladder. Metabolism occurs primarily by the liver and the majority excreted via the kidneys.

Clinical Signs of Chocolate Toxicity in Dogs
Chocolate toxicity can result in a wide range of clinical signs depending on the dose ingested. These can vary significantly based on each individual case, but can generally be categorised into one of the following three: gastrointestinal/mild clinical signs, neurological signs, and cardiovascular signs.
Gastrointestinal/Mild Signs
Hyperactivity & panting Restlessness or lethargy Vomiting or diarrhoea Polyuria or polydipsiaNeurological Signs
Hyperthermia Ataxia Tremors & seizures ComaCardiovascular Signs
Tachycardia (+/- bradycardia if severe) Cardiac arrhythmias Hypertension (+/- hypotension if severe) Respiratory failure if severeDiagnostics for Chocolate Toxicity in Dogs
A wide range of diagnostics are available to determine the impact of the toxin beyond the dose range. This can also be helpful if an unknown amount of chocolate is ingested to be able to guide treatment. Useful diagnostics include:
PCV/TS
Evaluate the patient’s hydration statusBlood Gas
Hyperlactataemia possible in shock or ictal/post-ictal presentation Electrolyte derangements possible due to vomiting and diarrhoea Hypokalaemia possible late in course of toxicity (from emesis and diuresis) Hypoglycaemia possible secondary to increased muscle activityECG
Evaluate if arrhythmias are present or develop Monitor treatment of arrhythmiasNon-Invasive Blood Pressure (NIBP)
Hypertension or hypotension presence, or development during course of intoxication If severely neurological, potential monitoring for Cushing’s Reflex (hypertension in presence of bradycardia)Pulse Oximetry
Presence of hypoxia and requirement of oxygen therapy in severely affected/neurological patients Easy continual monitor of heart rate if no ECG attached to patient (if arrhythmia present, may not read accurately)Urine Specific Gravity (USG)
Iso-hyposthenuria due to diuretic effect of methyxanthinesOptional Diagnostic Tests
Biochemistry
If high content ingested with delayed presentation, consider running to determine if evidence of concurrent pancreatitisUltrasound
If decontamination was unsuccessful can be used to determine if a ball of chocolate is in the stomach (this can rarely can occur, requiring surgical removal)Radiography
If presenting with signs of vomiting or seizure already and concerned of aspiration (e.g hypoxia, harsh lung sounds)Laboratory Testing
Methylxanthines may be detectable in serum or plasma up to 3-4 days post-ingestion and can be detected by external laboratory tests No in-house tests are able to detect
Treatment of Chocolate Toxicity in Dogs
Asymptomatic Patient – Outpatient Treatment
Can be considered when chocolate ingestion is recent and asymptomatic. May also include ingestion of mild but potentially toxic dose (e.g. gastrointestinal signs range – approx. 15-30mg/kg); or when owner declines further hospitalisation.
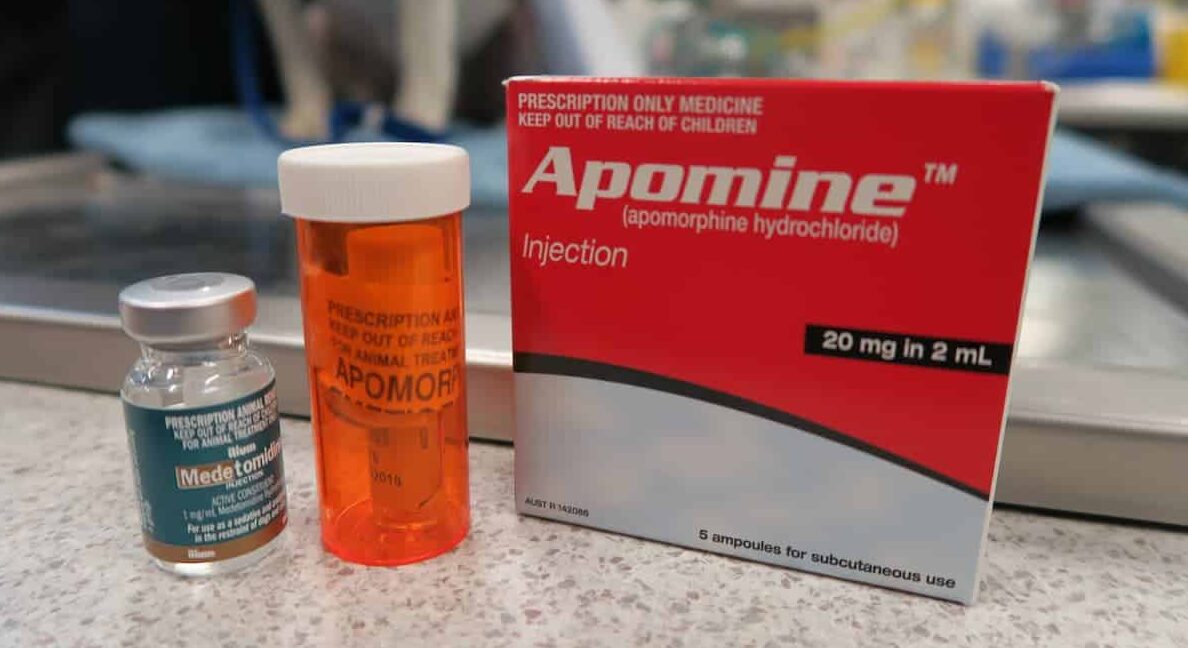
Emesis: Apomorphine tab into buccal mucosa or conjunctival sac• Up to 6hrs post-ingestion in stable patient (gastric emptying can be delayed)
• If time of ingestion unknown in stable patient
• NOT in unstable, neurological patient
• Reverse once reached bile-coloured vomitus
• Reversal: Metoclopramide 0.5mg/kg SC Activated Charcoal: to bind any remaining toxin within GIT
• Carbasorb (contains sorbitol – recommended cathartic to include): 5ml/kg PO q8
• Preferentially let the dog lick up, or syringe into dog’s mouth (avoiding aspiration)
• If needs to be fed with chicken, as it is a non-specific binding agent, the presence of chicken is theoretically reducing its effectiveness
• If dog licks up easily, consider sending home with pre-made syringe for O to feed in a bowl, DO NOT INSTRUCT TO SYRINGE FEED
• Charcoal powder: 1-4g/kg q8 into 1g/5ml water (used for subsequent doses, as cathartic is not indicated after first dose)
Asymptomatic Patient – Inpatient Treatment
Perform initial decontamination as above +/- Gastric lavage• If lethal dose ingested but emesis induction unsuccessful or not indicated (laryngeal paralysis, brachycephalic, history of aspiration pneumonia)
• Anaesthesia with ET tube (cuff inflated), pass lubricated stomach tube in lateral recumbency, flush with warm water solution, re-position patient to ensure all contents removed, when pulling out tube ensure end is kinked, it is not recommended to infuse with activated charcoal due to risk of aspiration Anti-nausea therapy
• If signs of vomiting or nausea on presentation or during hospitalisation
• Maropitant: 1mg/kg SC or IV q24
• Ondansetron 0.2-0.5mg/kg IV q8
• Metoclopramide CRI: 2mg/kg/day Intravenous fluid therapy
• To assist rehydration, cardiovascular system, optimize GFR to permit diuresis
• Dependent on animals requirement, if diuresis required without rehydration consider 1-1.5% x Maintenance of a balance solution
• Supplement for any electrolyte derangements (e.g. hypokalaemia) Urinary Catheterisation
• Consider for patients with high or lethal dose ingestion, delayed presentation to clinic, ineffective decontamination, clinical signs present already
• Reduces reabsorption through bladder mucosa, which prolongs clinical signs
• Place in conscious (+/- sedation) males, or anaesthetised females
Symptomatic Patient – Inpatient Treatment
Perform treatment as above except for emesis induction, which is contraindicated in clinically affected patients• Activated charcoal q8 for 2-3x doses (Theobromine half-life 17.5 hours) acceptable in stable, clinically affected patients (e.g gastrointestinal signs only, mild tachycardia)
Gastroprotectants to be considered to prevent mucosal irritation
• Esomeprazole 1mg/kg IV q8-12 Treatment for any cardiac disturbances
• Ventricular arrhythmias: Lignocaine 1-2 mg/kg IV bolus followed by 25-75ug/kg/min CRI• Maropitant: 1mg/kg SC or IV q24
• Hypertension/supraventricular tacchyarrhythmias: metoprolol 0.2mg/kg PO q12 (metoprolol is preferred over propranolol due to the potential of reduced methylxanthine clearance with propranolol; monitor for hypotension)
• Bradycardia: IV atropine 0.02 – 0.04 mg/kg IV or IM
• Hypotension: dobutamine CRI 1-20mcg/kg/min Treatment for any neurological disturbances
• Seizures: 0.5-1mg/kg IV Diazepam PRN +/- phenobarbitone or midazolam +/- propofol CRI
• Tremors: consider methocarbamol boluses 40-50mg/kg IV over 3-5mins PRN +/- CRI 10mg/kg/hr (do not exceed 330mg/kg/day)
• Severe uncontrollable seizure activity or comatose state: intubation and IV anaesthesia, considering half-life of toxin (4.5hrs for caffeine, 17.5 hours for theobrombine)

Costs, Risk Factors, and Prognosis
Hospitalisation time to expect is typically between 12 – 24 hours for most patients. This can occasionally be greater than 72 hours in severely affected animals due to theobromine half-life. Costs whilst hospitalized can range from $1000 – $2000 initially (depending on treatment), $300-600 for every 12hrs for stable patients, $500 – 800/12hrs for unstable but conscious patients, or up to ~$3000/24hrs for intubated patients.
Risk factors for chocolate toxicity in dogs includes young dogs due to their natural curiosity and small breed dogs, as they have a higher risk of consuming a large and potentially life-threatening dose. Other risks include:
Brachycephalic breeds, which have a greater risk of respiratory compromise and aspiration; Patients with prior episodes of acute or chronic pancreatitis (due to greater risk of pancreatitis developing); Animals on propranolol or steroids may have reduced clearance of methylxanthinesMost mild to moderate asymptomatic cases will have good to great prognosis if treatment is early and aggressive. Prognosis is approximately 50:50 if aspiration occurs secondarily (or lower if charcoal is aspirated). Prognosis will be poor to guarded if the patient presents with cluster seizures or in a comatose state.
With swift decontamination and appropriate response to a patient’s level of toxicity, whether symptomatic or asymptomatic, most cases of chocolate toxicity in dogs can be managed effectively. To be prepared for your next case, download our printable chocolate toxicity protocol PDF below and sign up to VetAPedia to access our library of clinical resources.
chocolate
Download Your Chocolate Toxicity Protocol
The post Chocolate Toxicity in Dogs – Clinical Protocol appeared first on Animal Emergency Australia.











