The application of artificial intelligence (AI) demands a judicious and data-driven strategy. Initial enthusiasm led to widespread adoption, but practical experience has highlighted the importance of aligning AI capabilities with specific operational needs. Healthcare organizations are grappling with complex revenue cycle management issues, stemming from evolving insurance reimbursement policies, rising patient financial burdens, and multifaceted […] The post Leveraging AI to Predict Patient Payment Behaviors appeared first on MailMyStatements.
The application of artificial intelligence (AI) demands a judicious and data-driven strategy. Initial enthusiasm led to widespread adoption, but practical experience has highlighted the importance of aligning AI capabilities with specific operational needs.
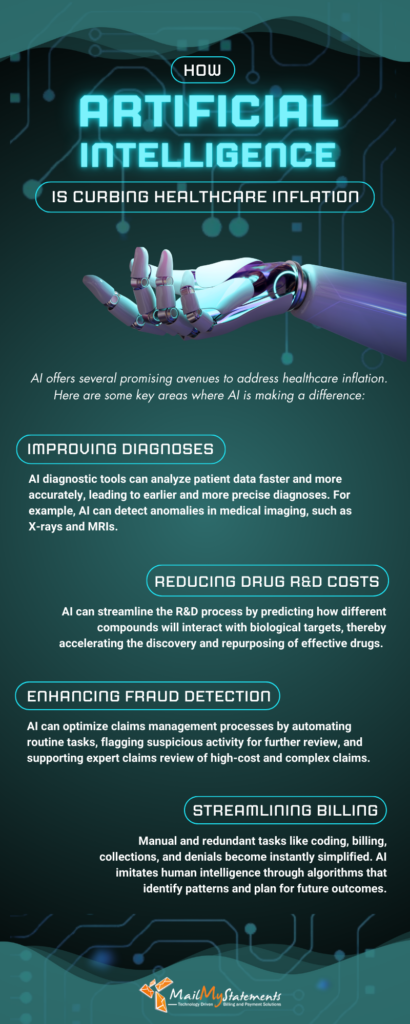
Healthcare organizations are grappling with complex revenue cycle management issues, stemming from evolving insurance reimbursement policies, rising patient financial burdens, and multifaceted payment plans, significantly complicating patient payment prediction and collection. While AI’s role in addressing healthcare inflation is understood, a critical inquiry persists: can AI leverage data analytics to optimize revenue cycles by accurately predicting patient payment behavior?
This article explores how AI-driven data models can be used to predict patient payment patterns, create smarter workflows, and ultimately shorten the revenue cycle. By leveraging AI, healthcare providers can forecast patient payment behaviors with unprecedented accuracy, paving the way for improved revenue cycle management.
The Current Complexity of Revenue Cycle Management
The financial landscape for healthcare providers has grown more complex in recent years. As of 2023, patient responsibility—out-of-pocket costs such as deductibles, copayments, and coinsurance—accounted for approximately 30% of provider revenue, up from just 10% a decade prior.
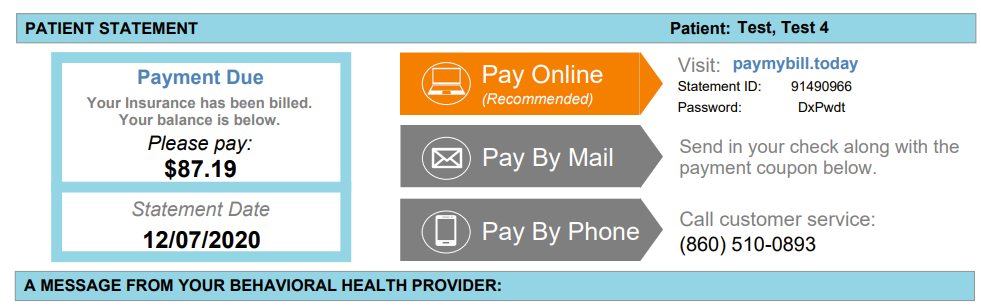
Compounding the issue are antiquated payment systems that rely on paper statements, along with manual processes to evaluate patient payment risks (if such risks are calculated at all). These outdated workflows may fail to optimize collections or identify red flags before they escalate.
AI technology, however, brings something new to the table—a predictive ability to assess and address financial risks before they materialize.
AI in Revenue Cycle Management
AI is used in revenue cycle management to apply advanced algorithms and data-driven models to analyze financial, behavioral, and operational data. In doing so, AI has the ability to identify patterns, trends, and probabilities that older, traditional processes may overlook. Unlike manual systems, AI learns and evolves over time, improving the accuracy of its predictions with each new piece of data it receives.
When it comes to predicting patient payment behaviors, AI leverages historical data like prior payment history, insurance coverage, and demographics to anticipate whether, how, and when a patient might pay. AI can then customize a payment plan, facilitate billing queries, and remind the patient of payments due.
How Healthcare Providers Can Use AI to Predict Patient Payment Behavior
AI uses multiple data points and advanced algorithms to paint a clearer picture of a patient’s likelihood to pay on time—or pay at all. Here’s how it works:
Analyze Past Payment Data
AI systems analyze past payments made by patients, looking at their timing, frequency, and amounts. This data is layered with demographic information, such as insurance coverage, income, and employment status, to identify patterns of behavior. AI may determine, for example, that a patient who has made consistent past payments but has a limited income may require an installment plan to stay on track.
Incorporate Real-Time Data
One of AI’s key strengths is its ability to integrate real-time inputs from disparate sources. For instance, sudden changes in a patient’s profile, like a denied claim, are flagged immediately. AI tools can immediately factor in such changes while recalibrating the likelihood of future payment and implement a solution right away.
Conduct Behavioral Modeling
AI uses behavioral analytics to assess factors such as response rates to reminders or interactions with customer service to predict the likelihood of patients making payments. For example, if data shows that text-message payment reminders result in faster compliance with patients who fall into certain age demographics, AI can prioritize that method for those patients, and de-prioritize it for others.
Apply Propensity-to-Pay Scoring
AI can produce a patient payment likelihood score, or propensity-to-pay score, which tells healthcare providers at a glance which patients are low-, medium-, or high-risk in terms of potential payment delays or defaults. Armed with this information, providers can focus their resources on high-risk cases while automating tasks for low-risk accounts.
4 Benefits of AI in Predicting Patient Payment Behaviors
Using AI’s predictive analytics to forecast patient payment behaviors has the following benefits:
1. Higher Recovery Rates
With accurate propensity-to-pay scores, healthcare organizations can better engage patients to offer payment plans to those with a high likelihood of payment default. AI’s predictive capabilities are more likely to keep overdue accounts from slipping through the cracks than other methods.
2. Smarter Staff Allocation
By categorizing patients based on their risk levels, revenue cycle teams have the ability to use their time and energy more efficiently. Higher-risk accounts may warrant personal outreach from billing staff, for example.
3. Improved Patient Experience
Predictive models enable providers to offer personalized payment options based on a patient’s financial ability and preferences. When providers can meet patients where they’re at and anticipate their needs, their willingness to pay improves.
4. More Accurate Revenue Planning
Forecasting payment behaviors allows providers to plan budgets and cash flow with greater accuracy. This equips financial managers to better allocate operational funds and strategize long-term investments.
Challenges and Considerations
Although the promise of AI in predicting patient payment patterns is exciting, there are some challenges to keep in mind:
Data Privacy
Because AI relies on large sets of patient data, compliance with data privacy regulations like HIPAA is critical. Healthcare providers and outside vendors must prioritize security and transparency in handling sensitive financial and personal information.
Integration with Existing Systems
Adopting AI requires integration with current electronic health records (EHR) and billing platforms. A disconnected solution may create more bottlenecks than efficiencies.
Avoiding Over-Reliance
While AI provides invaluable decision support, it cannot replace the work of human staff. Their personal oversight is still needed to ensure the ethical application of these tools and to address unique patient circumstances that algorithms cannot predict.
Using AI to Predict Patient Payment Behavior: The Present and the Future
Although the use of predictive analytics in patient billing is still in its infancy, organizations are already reaping the benefits of AI-enhanced billing processes. After experiencing success with using AI to automate insurance coverage discovery, Banner Health developed a predictive model to determine when write-offs are recommended for bad debt. This recommendation is based on the probability of payment and denial codes.
This example shows how AI-powered tools are reshaping the way healthcare handles revenue cycle management by giving providers a new tool to maintain financial stability and reduce wasted time. That said, the full potential of predictive AI lies ahead. Future advances in machine learning and increased integration into clinical systems will pave the way for more efficient revenue cycle management.
Final Thoughts
Get in touch with us today and learn more about how MailMyStatements’ BillingCycle Plus software can help streamline your patient billing and payment collection process with digital tools like eStatements, SMS text message payment alerts and reminders, and machine learning chatbots.
![]()
The post Leveraging AI to Predict Patient Payment Behaviors appeared first on MailMyStatements.